IVF 101
Feb 20, 2009
This post is meant to serve two purposes: 1) to help family and friends who have never been through in-vitro fertilization (IVF) to better understand the process and 2) to help me better process in my own mind what I am about to go through.
There are five main phases of the IVF process. The process is completed during the same amount of time it takes to complete a normal one-month menstrual cycle.
- Ovarian Stimulation
- Egg Retrieval
- Fertilization
- Embryo Culture
- Embryo Transfer
Ovarian Stimulation
During ovarian stimulation the ovaries are stimulated using powerful fertility drugs with the goal of having as many eggs as possible mature. Having as many eggs as possible mature is necessary because some may not fertilize at all while others will fail to develop normally after they are fertilized.
The ovarian stimulation drugs I will be on are Letrozol, Menopur and Follistim. While Letrozol is taken orally, the other two drugs must be administered through daily injections. Yes, IVF patients essentially become a pin cushion when it is all said and done!
I will be on a Step Down Protocol. This means that I will start out on very high dosages of these drugs (because our goal here is many mature eggs) and will step down on the dosage once we see how my ovaries are reacting and how many eggs they appear to be producing.
During ovarian stimulation my ovaries will be closely monitored by frequent ultrasounds.
There is a condition called Ovarian Hyperstimulation Syndrome (OHSS) which can occur during ovarian stimulation. I am at a higher risk for developing this condition because I am young, lean and have polycystic ovaries. The ultrasounds will also allow my doctor to watch for OHSS developing during ovarian stimulation. And I fully intend to have all my prayer warriors praying against OHSS!
I’m sure the stimulation drugs have all kinds of lovely side effects. However, I’ll just have to take what comes, knowing the side effects will only be temporary. Again, we will be praying against negative side effects!
Egg Retrieval
As the eggs mature I will have one last injection: an hCG injection. I had this injection during all three IUI cycles to induce ovulation. The purpose of an hCG injection during IVF is to mature the eggs even further before they are retrieved (instead of ovulated).
The egg retrieval procedure is performed in the surgical unit a floor below the infertility clinic. The procedure takes approximately 15 - 20 minutes.
Eggs are retrieved by a transvaginal ultrasound-guided aspiration procedure. Basically, during the procedure an ultrasound probe is inserted into the vagina to identify mature follicles. Then, a fine needle is guided through the vaginal wall and into the follicle where the egg is aspirated (retrieved) through the needle.
Ouch?!?! Don’t worry. I will be fully sedated throughout the whole procedure although I have to admit, I would love to witness the whole thing.
There are many variables that influence the number of eggs that will be retrieved from any one woman.
Fertilization
Shortly after egg retrieval, eggs are placed with motile sperm in a petri-dish (hence the name, in-vitro fertilization). And then, well, it’s quite simple. The number of eggs that successfully fertilize is completely up to God, since He is the creator of life.
Prayer warriors, this will be a HUGE praying day!
Depending on the quality and quantity of the sperm sample a procedure called intracytoplasmic sperm injection (ICSI) may be performed. During ICSI, a single sperm is injected directly into the egg, however, fertilization is still not a guarantee because, once again, fertilization is God’s business. God is the creator of life!
The day after the egg retrieval I will receive a report on how many eggs fertilized successfully. Fertilization is documented by the presence of two nuclei. One nucleus is from the sperm and one is from the egg.
Embryo Culture: A Three to Five Day Process
Day 1: After fertilization, the nuclei from the egg and sperm fuse and the cellular division process of the newly created embryo begins.
Day 2: The embryos are carefully monitored for growth and proper cell division. The embryos are growing from a two-cell embryo to a four-cell embryo.
Day 3: The embryos are in the six to eight-cell stage now. Depending on the number of embryos, day three may be the transfer day (will explain what “transfer” is below.) If three or more eight-cell embryos are present, a 5-day transfer is very possible. Five-day transfers allows for better embryo selection since some of the embryos will not progress beyond the eight-cell stage. The decision on whether to do a 3-day or 5-day transfer is largely dependant on the number of embryos present and their quality.
Day 4: Eight-cell embryos that continue to grow and develop will now be at the morula stage (15-32 cell embryo).
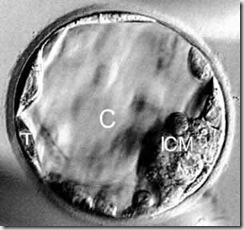
Day 5: The embryos who make it to day five, form a cavity called the blastocoel (which is why the embryo can now be called a blastocyst). s of a blastocyst organize themselves into outer cells, which will form the placenta (labeled “T” in the picture below), and inner cells, which will form the baby (labeled ICM). The blastocoel cavity in the center is labeled “C”.
Everyone going through IVF prays for embryos that are strong enough to make it to a 5-day transfer. Prayer warriors, we will be praying the same!
(Click here to see one of my blogger friend’s blastocyst picture. She just recently went through IVF, had 2 perfect blastocysts transfered and is now 7 weeks pregnant with TWINS!)
In summary, there are three critical development points that must occur if a 5-day transfer is to take place:
- Fertilization
- Four to eight-cell embryo stage
- Morula to Blastocyst Stage
Embryos are “graded” using a numeric grading system with a Grade 1 embryo being the best and a Grade 4 embryo being the worst. It is important to know that the grade an embryo receives is no indication whatsoever about whether it will become a healthy or unhealthy baby. The grade is meant to only give doctors and their patients a means by which to measure the viability of any one embryo. In other words, a Grade 1 embryo has a much higher chance of actually implanting into the uterus and becoming a viable pregnancy whereas a Grade 4 embryo’s chance of becoming a viable pregnancy is not impossible, but very unlikely.
Obviously, we will be praying for many Grade 1 embryos that can make it to a 5-day transfer!
Embryo Transfer
During the embryo transfer, the doctor inserts a catheter through the cervix into the uterus and transfers one or more embryos. The embryo(s) is/are strategically transferred to the particular place an embryo would naturally implant in the uterus. If the embryo continues to develop in the uterus, it will hatch from the egg’s outer layer and implant into the uterine lining approximately six to ten days after the egg retrieval.
Depending on a woman’s age and the viability (grade) of her embryos, the American Society for Reproductive Medicine recommends transferring one to three embryos.
Cryopreservation – What to do with any “left over” embryos
Any remaining embryos following the embryo transfer can be frozen for future use.
This is perhaps the most controversial aspect of the in-vitro fertilization process. I believe the only unethical aspect of the cryopreservation process is discarding left-over embryos because “we are done having children”. I also believe that the moment sperm and egg unite, new life is formed.
In my particular situation, it will be a miracle if we have any left-over embryos. Because of my endometriosis we really do not have a clear picture of what my egg quality really is. We know that having had endometriosis declines egg quality sooner. Quite frankly, we will be praying for enough eggs and enough quality embryos for just this one cycle. Any “extras” at the end will be considered an extra blessing from God.
If there are any “extras” and the first cycle of IVF fails, we will not have to go through any of the first four steps described in this post. A certain number of frozen embryos will be “unfrozen” and then transferred into my uterus at a fifth of the cost that this first, fresh IVF cycle.
Since childhood, it has always been my dream to one day be the mother to four children. Consequentially, being faced with the decision to discard left over embryos will never come into play with us. To have four children through IVF, an extremely large amount of good quality embryos would have to be present; which is why, for now, if this IVF cycle results in Dave and me having one biological child, I will consider that baby my miracle baby.
*****
There really is so much more I could have included in this post. But I chose to stick with the basics so as to not make this post any longer than it already is.
- Elaine